Advancing Patient Safety in Africa:
Implementing the Global Patient Safety Action Plan (GPSAP)
Background and Overview
Patient safety is recognized globally as both a health priority and a cornerstone of high-quality care. Despite major advances in medical science and healthcare delivery, millions of patients continue to experience avoidable harm in the course of receiving treatment. The World Health Organization (WHO) ranks unsafe care among the top ten causes of death and disability worldwide.
In response, WHO launched the Global Patient Safety Action Plan 2021–2030 (GPSAP) in 2021, a strategic framework designed to eliminate avoidable harm in healthcare. Its vision is clear: a world in which no one is harmed in health care, and every patient receives safe and respectful care, every time, everywhere. The GPSAP calls on countries to adopt system-level approaches to embed safety into policies, leadership, culture, and practice.
The urgency of this framework is particularly evident in low- and middle-income countries (LMICs), where risks are disproportionately high. Evidence shows that poor-quality care causes more deaths in LMICs than lack of access, with an estimated eight million excess deaths annually linked to substandard healthcare. WHO’s Global Patient Safety Report 2024 highlighted this reality, stressing that while progress has been made, persistent gaps continue to undermine safe care delivery.
To address these disparities, WHO has issued global and regional calls to action encouraging member states to integrate GPSAP into their national health policies. Platforms such as the WHO Regional Committee for Africa have endorsed this approach, urging countries to design context-specific solutions and adopt sustainable strategies for patient safety.
The Seven Strategic Objectives of GPSAP Make zero avoidable harm to patients a state of mind and a rule of engagement in the planning and delivery of healthcare everywhere
-
- Patient safety must be seen as a non-negotiable moral and professional responsibility. Embedding this value ensures that safety is prioritized in every interaction between patients and health workers, across all levels of healthcare systems.
- Build high-reliability health systems and health organizations that protect patients daily from harm
The goal is to move from reactive, fragmented safety responses toward systems that are proactive, resilient, and capable of preventing harm before it occurs. High-reliability systems anticipate risks, adapt to challenges, and maintain consistent standards of safe care. - Assure the safety of every clinical process
Clinical areas with high risk, such as medication use, infection prevention, maternal and newborn care, and surgery, must be systematically addressed. Standardizing and improving these processes reduces the likelihood of errors and protects patients from preventable harm. - Engage and empower patients and families to help and support the journey to safer healthcare
Patients are not passive recipients of care; they are partners in ensuring safety. By involving patients and families in decision-making, co-design, and feedback, health systems can strengthen trust, improve communication, and better detect risks. - Inspire, educate, and protect health workers to contribute to the design and delivery of safe care systems
Patient safety starts with health workers. Yet, many training programs still overlook system risks, human factors, and teamwork. By integrating patient safety into education, protecting health workers’ well-being, and fostering leadership, we can build safer, more reliable health systems across Africa. - Ensure a constant flow of information and knowledge to drive the mitigation of risk, a reduction in levels of avoidable harm, and improvements in the safety of care
Incident reporting, surveillance, and health information systems are vital for identifying risks and guiding corrective action. Turning data into insights ensures that health systems not only capture information but also use it to continuously improve safety. - Develop and sustain multisectoral and multinational synergy, partnership and solidarity to improve patient safety and quality of care
Strategic Objective 7 emphasizes building multisectoral and multinational partnerships to embed patient safety across all levels of healthcare. Stronger collaboration spanning governments, professional bodies, civil society, patient advocates, and global organizations can transform outcomes. These partnerships not only reduce avoidable harm but also institutionalize patient safety as a cornerstone of universal health coverage.
- Patient safety must be seen as a non-negotiable moral and professional responsibility. Embedding this value ensures that safety is prioritized in every interaction between patients and health workers, across all levels of healthcare systems.
Learning from the Philippines
The Philippines has made significant strides in implementing the Global Patient Safety Action Plan (GPSAP) 2021–2030, embedding patient safety into national health policies and aligning it with the broader Universal Health Care framework. The country’s approach emphasizes preventing avoidable harm in prevention, diagnosis, treatment, and follow-up, while building a culture where reporting is valued and not punished. A revised National Policy on Patient Safety outlines clear roles and responsibilities for safety officers and committees, ensuring accountability and structured action across both public and private facilities. This institutionalization of patient safety is seen as essential for protecting vulnerable populations and strengthening overall health system performance.
To operationalize the policy, a National Patient Safety Program Strategic Plan was developed that envisions all health facilities embracing a culture of safety by 2028. Its strategies include empowering leaders as champions, creating standards, expanding access to training, promoting advocacy, and strengthening networks and monitoring systems. Notable initiatives include the designation of Patient Safety Officers, online training courses accessible through the Department of Health’s eLearning Academy, and tailored adoption of WHO tools such as the Surgical Safety Checklist and the Safe Childbirth Checklist. These tools have been adapted for local contexts, tested in facilities, and formally integrated into national practice.
The Philippines has also prioritized measurement and accountability. Patient Safety Indicators (PSIs) were introduced to monitor areas such as patient identification, effective communication, safe surgery, medication safety, fall prevention, and infection prevention. These indicators are now embedded into the national Health Facility Profiling System, with facilities required to submit data annually. This ensures that safety performance contributes directly to hospital scorecards and even influences performance-based financial support, thereby incentivizing continuous improvement.
Beyond policies and tools, the Philippines has cultivated a strong culture of engagement and advocacy. Regular celebration of World Patient Safety Day mobilizes health facilities and communities to champion safety. National conferences and summits, such as the recent 7th Global Ministerial Summit on Patient Safety, have provided platforms for showcasing best practices, advancing regional collaboration, and aligning safety with pressing global challenges, including climate resilience and digital transformation. A key outcome of this summit was the Mandaluyong Declaration on Patient Safety, a landmark commitment to shared learning, transparency, and people-centered, climate-resilient healthcare systems.
The Philippine experience underscores several lessons. Policies alone are insufficient without funding, implementation, and accountability mechanisms. Fear of blame and fragmented systems still limit open reporting, pointing to the need for legal protections and independent oversight. At the same time, innovation is advancing: new manuals, online training modules, AI-assisted diagnostics, and psychological safety initiatives such as TeamSTEPPS are being introduced to strengthen resilience and reduce risks. Taken together, these measures highlight how patient safety can be institutionalized at scale, with governance, culture, and capacity working in tandem to reduce harm and build trust in healthcare.
Implementing the GPSAP in African Countries
Kenya has embedded patient safety as a central pillar of its health agenda, transitioning responsibility from the Ministry of Health to the Kenya National Public Health Institute. A national patient safety policy and action plan was developed in 2021, and a Quality of Care and Safety Bill is currently under discussion to strengthen the legal framework. The country also observes World Patient Safety Day annually to keep awareness high. Recently, Kenya launched a patient safety technical working group focused on thematic areas such as medication safety and infection prevention and control, and has consistently adopted WHO tools like the Surgical Safety Checklist and Safe Childbirth Checklist.
On workforce and engagement, Kenya has created a patient safety training package integrated into the MOH Virtual Academy, with continuing professional development (CPD) credits under discussion to encourage uptake. Patients and patient safety advocates were engaged during policy development and are now part of the new technical working group. Research and indicator monitoring remain at early stages, with pilots in eight facilities across four regions facing challenges due to blame culture. Kenya has also built strong collaborations, partnering with organizations like ACQUIRE, COFPAK, and the Society for Quality in Healthcare, as well as regional and global networks, including a community of practice with Ethiopia in IPC and AMR.
In Malawi, patient safety is integrated into broader quality strategies rather than existing as a standalone policy. It is prioritized in both the national quality policy and the overarching Health Sector Strategic Plan III, which runs until 2030. Client safety is among seven national priorities, with a focus on safeguarding against malpractice, implementing patient safety standards, and scaling IPC/WASH standards and antimicrobial stewardship. The star rating program, measuring facilities from one to five stars based on adherence to safety standards, has become a cornerstone, fostering a sense of competition and continuous improvement.
Malawi has extended IPC and WASH interventions to nearly all facilities, reinforced by experiences with COVID-19, cholera, and Mpox. Over 190 facilities now participate in the star rating system, supported by a national patient safety focal person and a hospital ombudsman role to gather client feedback. Innovations such as the star rating system have instilled pride and a sense of progress, though challenges remain. Many facilities lack formal patient safety policies, patient safety indicators are not fully integrated into health information systems, and most initiatives are concentrated in secondary and tertiary facilities. Opportunities exist in decentralizing efforts to primary care, standardizing training, and learning from regional peers on sustainable standards and indicator integration.
Ethiopia has progressed from implicit efforts to explicit patient safety strategies, beginning with a national quality and safety strategy from 2016-2020 and followed by a second national strategy (2021-2025) prioritizing safety as two of its five objectives. A dedicated quality and safety structure exists at national and regional levels, supported by a national patient safety guideline that shapes ongoing initiatives. The country has also introduced IPC policies, monitoring and evaluation tools, and hospital-acquired infection surveillance systems.
Implementation includes clinical process improvements such as a national preoperative guideline, safe surgery checklist utilization, and IPC and AMR programs. Legal measures require healthcare professionals to report incidents, while accreditation programs for hospitals and health centers are in development. Patient and family engagement remains limited, though patients’ associations are represented in national committees. Education efforts include in-service training, a master’s program in quality and safety, and pre-service integration of patient safety into curricula. While incident reporting guidelines exist, implementation gaps remain, and Ethiopia is working to strengthen hub hospitals as centers of excellence in safety.
Nigeria has adopted the GPSAP objectives, with progress driven by a national coordination unit for patient safety within the Federal Ministry of Health. A patient safety strategy was developed between 2021 and 2023, supported by a dedicated budget line for safety programs. The government has initiated an incident reporting system at the national level, while robust clinical governance, IPC programs, and medication safety initiatives have been cascaded down to tertiary institutions. Standards exist for primary health care facilities, with work ongoing for tertiary-level standards.
At the hospital level, structures such as QI teams, M&M reviews, clinical audits, and protocols are in place, with some facilities using incident reporting tools. However, a weak reporting culture persists due to fear of blame and lack of legal protections. Data for learning is still limited, and sustainable financing remains a major challenge. Planned reforms include incorporating patient safety more strongly into the National Health Act, strengthening incident reporting, and sustaining engagement with both frontline professionals and patients. Patient voices have been included in guideline development, marking an important step toward participatory safety culture.
Ghana established a Quality Management Unit in 2017 alongside its first national healthcare quality strategy, embedding patient safety as a core element. This was followed by a dedicated national patient safety strategy (2021-2023), complementing a revised quality strategy for 2024-2030. Patient safety is supported by a separate IPC strategy developed after COVID-19, and regulation is reinforced by distinct authorities that license facilities and oversee medicines, food, and medical equipment. Professional regulators have also integrated patient safety into CPD requirements and pre-service curricula, including specialized IPC training programs for nurses and midwives.
Field innovations include the establishment of national quality and safety committees, regional learning platforms, and adoption of the WHO Surgical Safety Checklist to reduce surgical harm. Patient and community engagement is central: Ghana hosts annual patient safety conferences, conducts mandatory client satisfaction surveys every six months, and uses community scorecards to capture service-user feedback at the lowest levels. Partnerships with donors such as USAID have supported this work, though sustaining momentum post-donor funding is a challenge. Looking forward, Ghana has called for stronger cross-country platforms for shared learning and regional peer support.
Tanzania is reviewing its national health sector policy to prioritize patient safety in alignment with the GPSAP. A national patient safety guideline and a framework for safe surgery are in the final stages of approval, alongside the AFYA Supportive Supervision tool (AfyaSS), which embeds safety standards into system assessments. The Maternal and Perinatal Death Surveillance and Response (MPDSR) mechanism exemplifies a no-blame, learning-focused approach, requiring maternal deaths to be reported within 24 hours and discussed at facility, district, and national levels. This has contributed to reducing maternal mortality rates from 553 to 104 per 100,000 live births.
Other innovations include tumor boards in referral hospitals to ensure safe cancer care and vigilance systems for reporting adverse drug reactions. Blood safety is reinforced through eight zonal centers, seven of which are accredited, ensuring screened and safe transfusions. Challenges remain, but Tanzania’s integration of safety into both policy and daily practice illustrates how structured systems can yield measurable improvements, especially in maternal health outcomes.
Uganda does not yet have a dedicated patient safety strategy but is laying the groundwork through projects supported by WHO and JICA. Baseline studies have mapped the current situation, and a national steering committee has been formed within the Ministry of Health. Patient safety efforts are being introduced through a stepwise model: facilities first adopt workplace improvement practices using the 5S approach, then build QI capacity through Kaizen, and finally integrate safety initiatives. This gradual approach is designed to foster organic growth and ownership, recognizing the entrenched blame culture and weak clinician engagement as barriers to open reporting.
Structures for QI are already strong, with QI teams established in all facilities and a national framework in place. Uganda is piloting a “hospital safety report” system, deliberately framed with positive language rather than “incident reporting”, to encourage learning rather than blame. Draft guidelines for this system are under development, with national rollout planned. Patient feedback mechanisms are more advanced, with daily client feedback systems and monthly reporting targets in place, but integration of patient safety into the national QI framework remains a priority. Uganda’s focus is now on creating a unified national program that consolidates fragmented efforts and ensures data-driven decision-making across all facilities.
Key Themes Across African Country Experiences
There is a focus on integration of patient safety into national health and quality strategies. African countries are embedding patient safety within broader health sector and quality policies, as well as developing dedicated national patient safety strategies. This demonstrates two pathways to aligning with the Global Patient Safety Action Plan; either through standalone strategies or by embedding safety within wider health reforms. Both approaches show progress but highlight the importance of strong policy anchoring as the foundation for implementation.
There is a growing emphasis on establishing legal and regulatory frameworks for patient safety. Kenya, Ghana, and Tanzania are advancing laws, policies, and guidelines designed to strengthen accountability and align national systems with global standards. These efforts show that long-term progress depends on enforceable structures that go beyond programmatic initiatives.
There is also a strong focus on adopting and adapting WHO tools and global standards. Ethiopia has implemented national preoperative guidelines and surveillance systems, while Ghana has integrated the WHO Surgical Safety and Safe Childbirth Checklists into practice. By tailoring global resources to local contexts, countries are creating safer systems and promoting greater consistency across healthcare facilities.
There is increasing attention on capacity building and workforce development. Kenya, Ghana, and Ethiopia have integrated patient safety into both pre-service and in-service training, while Malawi has identified the need for standardized materials. Uganda emphasized gradual cultural change as a way to build awareness and ownership. These experiences point to the importance of embedding safety into professional development at every level of the health system.
However, a persistent challenge still lies in building a culture of incident reporting. Fear of blame and limited legal protections continue to discourage health workers from reporting errors, as acknowledged in Kenya, Uganda, and Nigeria. Some innovations, such as Uganda’s “hospital safety report” approach, are helping to shift perceptions, but reporting systems remain fragile and underused across much of the continent.
Post-Presentation Discussions
The discussion underscored a strong appetite for shared learning across countries. Participants highlighted the importance of connecting policies with frontline realities and emphasized that patient safety requires not only technical tools but also disciplined practices, accountability, and continuous professional behavior. Online reflections from across the continent pointed to the value of these exchanges in strengthening collective action and ensuring that patient safety is not left behind in broader health reforms.
Key themes raised in the Q&A centered on how to align safety with incentives, maintain objectivity in quality assessments, and foster cultures of learning rather than blame. Examples included linking hospital performance to budget allocations through scorecards, applying star-rating systems to encourage competition and adherence to standards, and adopting “no name” reporting to focus on system gaps rather than individuals.
Sustaining the Global Patient Safety Action Plan in Africa
The momentum around patient safety in Africa points to countries embedding safety into policies, laws, and quality strategies while piloting practical tools such as star-rating systems, hospital scorecards, and adapted WHO checklists. These efforts show that patient safety is no longer an abstract concept but a growing movement shaping how care is delivered and experienced.
Yet challenges remain. Weak incident reporting systems, limited legal protections, and the persistence of blame cultures continue to slow progress. The GPSAP’s call for resilient systems, empowered health workers, and engaged patients provides the framework needed to address these gaps. If African countries sustain their current trajectory, they will not only reduce avoidable harm but also create health systems that are safer, more trusted, and more resilient for future generations.
FOR FURTHER READING
- World Health Organization. (2024). Global Patient Safety Report 2024. https://www.who.int/publications/i/item/9789240095458
- World Health Organization. (2021a). Global Patient Safety Action Plan 2021–2030: Towards Eliminating Avoidable Harm in Health Care. https://www.who.int/publications/i/item/9789240032705
- World Health Organization. (2021c). Global Patient Safety Action Plan 2021–2030: An Overview. https://apps.who.int/gb/MSPI/pdf_files/2022/09/Item2_20-09v2.pdf
- Kruk, M. E., et al. (2018). High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health, 6(11), e1196–e1252. https://doi.org/10.1016/S2214-109X(18)30386-3
- World Health Organization. (2021b). Global Action on Patient Safety: WHA74(13). https://apps.who.int/gb/ebwha/pdf_files/WHA74/A74(13)-en.pdf
- World Health Organization Regional Office for Africa. (2020). Regional Committee for Africa: Seventieth Session Report. https://iris.who.int/bitstream/handle/10665/333998/AFR-RC70-14-eng.pdf
Key Session Highlights
Patient Safety as a Core Health Priority
Patient safety is moving from an abstract principle to a central pillar of health policy, with countries embedding it into national health strategies, quality frameworks, and sector reforms to align with the Global Patient Safety Action Plan (GPSAP).
Building High-Reliability Health Systems
There is a strong shift from fragmented, reactive safety measures toward resilient systems that anticipate risks, adapt to challenges, and sustain safe care as a daily practice.
Legal and Regulatory Anchoring
Laws, guidelines, and regulatory frameworks are being advanced in African countries to institutionalize safety and ensure accountability beyond program cycles.
Incentives and Accountability Mechanisms
Tools such as star-rating systems, hospital scorecards, and performance-linked financing are emerging as levers to improve adherence to safety standards and sustain commitment at the facility level
Moving Toward Sustainable Systems
While donor support and pilots have catalyzed change, sustainability will depend on institutionalizing safety into budgets, laws, and everyday clinical practice, ensuring long-term resilience and trust in care.
Multisectoral and Cross-Country Collaboration
Partnerships across governments, civil society, professional bodies, and global organizations are proving essential. Shared learning platforms and regional exchanges are accelerating collective progress.
quotes from the keynote speakers and panelists
Key Session Takeaways
What the WHO Global Patient Safety Action Plan (2021–2030) is
Key Takeaways
1 It aligns efforts across hospitals, patient care, and national policy to ensure consistency in patient safety.
2 The plan emphasizes collective responsibility, engaging all stakeholders, including healthcare workers.
3 Its success depends on translating strategy into action and measuring whether desired goals are being met.
How the Philippines Is Implementing Its Program-Specific Strategic Plan
Key Takeaways
1 A clear national roadmap guides patient safety efforts, covering planning, financing, implementation, and monitoring.
2 Building a culture of safety is central.
3 Collaboration, advocacy, and partnerships are key drivers of patient and worker safety.
How The Philippines Is Conducting Stakeholder Engagement In The Implementation Of ItsPatient Safety Program
Key Takeaways
Broad stakeholder engagement ensures that patient safety policies reflect multiple perspectives.
Including patient organizations amplifies the voice of those most directly impacted by care.
Collaboration with professional organizations and academia strengthens technical credibility.
How The Philippines Is Institutionalizing Its Patient Safety Program
Key Takeaways
1 National policies provide a strong foundation for consistent patient safety practices across facilities.
2 A no-blame culture encourages open reporting, learning, and continuous improvement.
3 Embedding patient safety across all levels of care protects vulnerable populations and strengthens equity.
Kenya’s Progress In Patient Safety: Policy, Systems And Healthcare Worker Training
Key Takeaways
1 Kenya has developed a national patient safety policy and action plan, with a quality of care and safety bill in progress.
2 Patient safety technical working groups have been launched, focusing on thematic areas like medication safety and IPC.
3 Sustained collaboration with regulatory bodies is needed to ensure CPD-linked patient safety training is widely adopted.
Nigeria’s National-Level Intervention on Patient Safety
Key Takeaways
1 Nigeria finalized a national patient safety document between 2021 and 2023 to guide interventions.
2 Provisions for safe medical equipment and healthcare worker training are part of ongoing budgeted activities.
3 A national incident reporting system is being developed to improve learning and accountability.
Ethiopia’s Progress In Patient Safety: Healthcare Worker Training
Key Takeaways
1 Ethiopia has developed in-service training programs to improve healthcare workers’ skills in quality and patient safety.
2 Guidelines for incident reporting have been established, strengthening accountability and learning systems.
3 Improvement area: Incident reporting systems need stronger implementation and uptake to ensure meaningful impact.
How Malawi Is Implementing The Global Safety Action Plan
Key Takeaways
1 Malawi integrates patient safety into its National Health Sector Strategic Plan III, prioritizing quality of care and client safety.
2 Patient safety standards are embedded into national quality of care standards, creating consistency across facilities.
3 Facilities are assessed on a 1–5 star rating system, linking performance directly to adherence to safety standards
How Tanzania Has Implemented A No-Name Policy On Error Reporting
Key Takeaways
2 Clear processes ensure accountability while avoiding unnecessary stigmatization of staff.
3 A no-name policy shifts focus from individual blame to system-level learning and improvement.
How Tanzania Reducing Maternal Mortality Rate
Key Takeaways
2 Clear guidelines and frameworks, such as for safe surgery, provide structure for reducing avoidable harm.
3 Rapid reporting and review mechanisms turn adverse events into opportunities for learning and prevention.
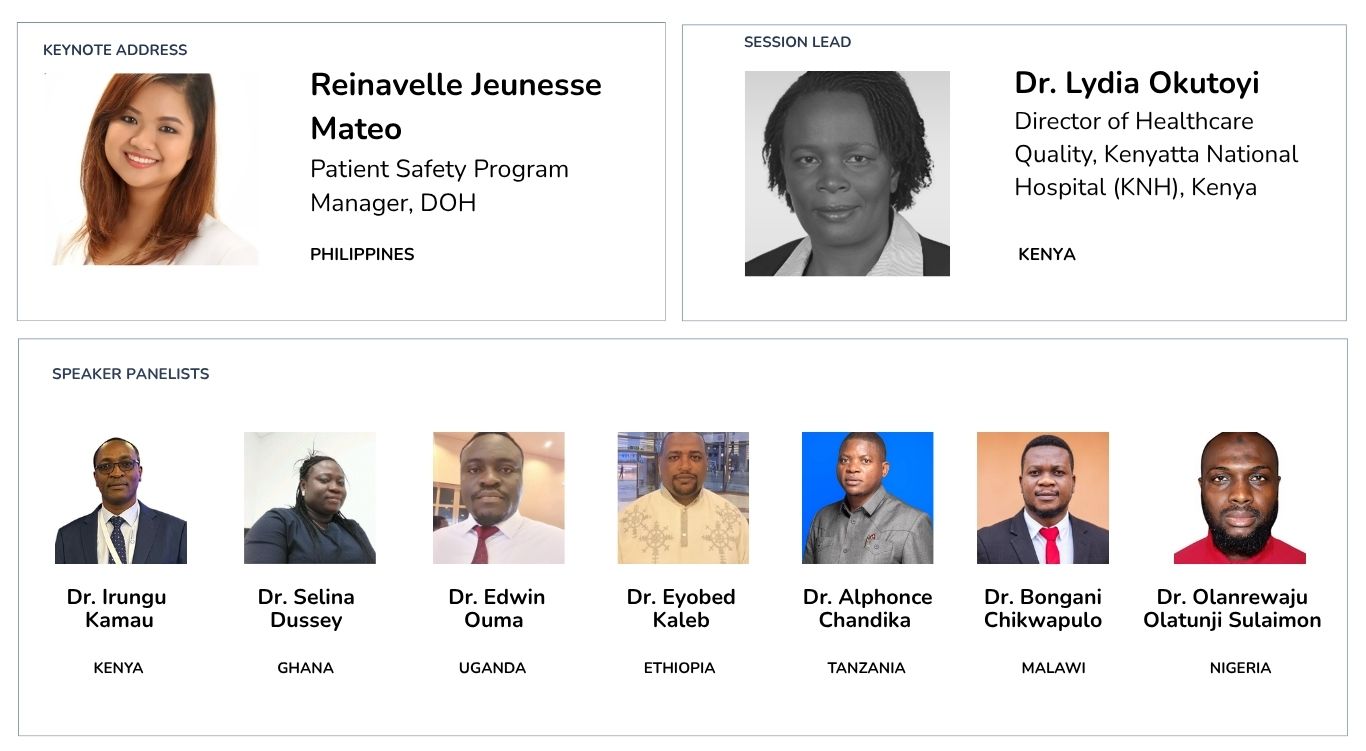
Live Recording, Speakers and Panelists
Advancing Patient Safety in Africa: Implementing the Global Patient Safety Action Plan (GPSAP)
ACQUIRE’s annual QI Leadership Forum is a continent-wide peer-learning platform on Patient Safety and Quality Improvement Practices in Africa. At ACQUIRE, we believe that improvement is a collective journey.
Join us in working towards more responsive, data-led health systems across Africa.
Email us: [email protected]
Connect with us on our social media platforms: